In today’s fast-paced medical environment, gas analyzers stand guard over patient safety, therapy optimization, and
compliance. They deliver real-time insights on oxygen, carbon dioxide, and anesthetic concentrations. By doing so, they prevent hypoxia, reduce overdose risks, and streamline treatment protocols. Moreover, they support clinical teams with data-driven decisions at every care stage.

(Patient, therapy, and compliance in healthcare)
Clinicians can’t afford a guess when they adjust ventilators, deliver anesthesia, or diagnose metabolic imbalances. Gas analyzers fill that gap by measuring:
- End-tidal carbon dioxide (CO₂) for ventilation accuracy
- Inspired Oxygen (O₂) for oxygen therapy
- Blood gas metrics for acid-base balance
Consequently, gas analyzers boost treatment precision and patient outcomes.
Moreover, regulatory bodies demand continuous quality checks on medical gas systems. NFPA 99 sets purity and monitoring rules. Centers for Medicare & Medicaid Services (CMS) and Food and Drug Administration (FDA) require documented gas analyzers performance to meet safety standards. As a result, hospitals integrate gas analyzers into workflows, ensuring audits and inspections run smoothly.
What Are the Core Clinical Applications of Gas Analyzers in Healthcare?
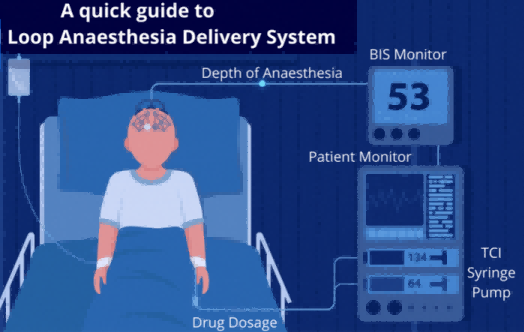
1. Anesthesia Delivery & Monitoring
(Anesthesia Delivery)
Firstly, gas analyzers deliver real-time readings of oxygen, carbon dioxide, and volatile anesthetics. This data lets anesthesiologists adjust anesthesia depth instantly. By monitoring inspired and expired concentrations, teams prevent patient awareness and overdose. As a result, clinicians maintain optimal sedation levels throughout surgery.
2. Respiratory Therapy & Critical Care

(respiratory-therapy)
Next, in critical care, analyzers guide ventilator settings via end-tidal CO₂ and FiO₂ feedback. This loop enhances breathing support for ARDS, COPD, and asthma patients. Clinicians track EtCO₂ trends to avoid hypo–or hyperventilation. Meanwhile, FiO₂ measurements ensure precise oxygen delivery. Consequently, therapy becomes more targeted and responsive to patient needs.
3. Diagnostic Breath Analysis
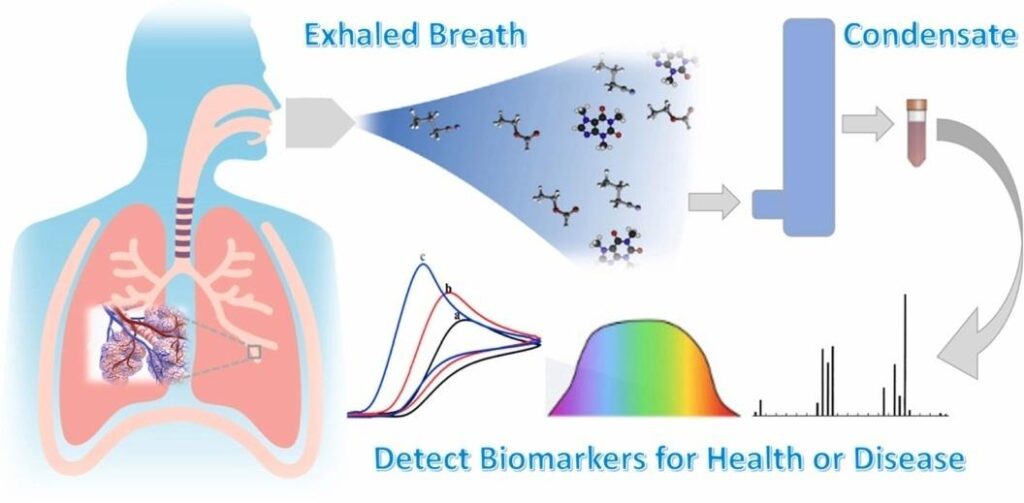
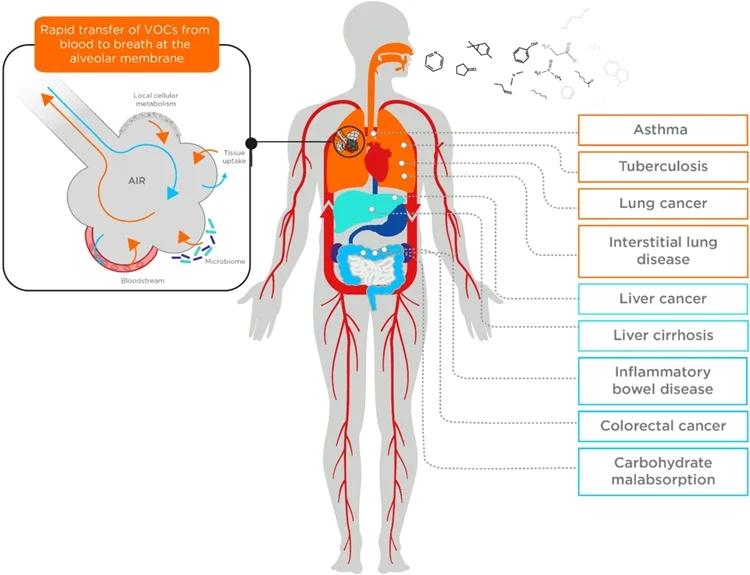
(Biomaker breath)
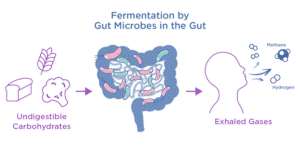
Additionally, gas analyzers transform diagnostics through blood gas and breath biomarker testing. They measure pH, PaO₂, and PaCO₂ for acid-base balance. Also, non-invasive breath tests detect exhaled nitric oxide and VOCs in asthma or infection screening. Furthermore, methane measurement helps diagnose constipation and SIBO by tracking gut microbial activity. Thus, breath analysis offers rapid, painless insights into patient health.
4. Medical–Gas Supply Quality Assurance
Finally, ensuring gas purity is vital for safe care. Quality monitors verify oxygen, nitrous oxide, and medical air purity. Gas analyzers detect cross-contamination and pipeline leaks in real time. As a result, teams meet Pharmacopeia standards and pass audits with confidence. Ultimately, supply assurance safeguards every breath a patient takes.
Which Key Gases Do Gas Analyzers Monitor in Healthcare?
–Oxygen (O₂):
Oxygen remains the cornerstone of respiratory monitoring. Gas analyzers measure FiO₂ and PaO₂ to confirm adequate tissue oxygenation and guide ventilator settings. Clinicians adjust therapy based on real-time O₂ levels. Accurate O₂ monitoring guides supplemental oxygen delivery and helps prevent hypoxia.
–Carbon Dioxide (CO₂):
Carbon dioxide monitoring via capnography tracks EtCO₂ and arterial PaCO₂, reflecting ventilation adequacy and metabolic status. Real-time CO₂ waveforms help detect hypoventilation or airway obstruction instantly. Clinicians rely on CO₂ trends to ensure proper respiratory function and patient stability.
–Nitrous Oxide (N₂O) & Other Anesthetic Agents:
Nitrous oxide and volatile anesthetics ensure balanced sedation and prevent awareness. Gas monitors quantify inspired and expired N₂O, sevoflurane, isoflurane, desflurane, and others breath by breath. This data lets anesthesiologists titrate minimal alveolar concentration (MAC) precisely. Consequently, teams maintain optimal sedation depth and minimize cardio respiratory side effects. Effective volatile-agent monitoring also reduces environmental contamination in operating rooms.
–Carbon Monoxide (CO) & Methane (CH₄):
CO and CH₄ analyzers safeguard gas-supply integrity. CO detection at ppm levels alerts teams to leaks or pipeline contamination. Likewise, CH₄ sensors identify trace methane in medical air, preventing equipment damage and false diagnostics. By integrating these analyzers into pipeline systems, hospitals maintain gas purity and patient safety. Real-time CO and CH₄ alarms support immediate corrective actions.
–Volatile Organic Compounds (VOCs):
VOCs cover anesthetic vapors and breath diagnostic markers. Clinicians analyze methane, nitric oxide, and VOCs at trace levels for non-invasive disease screening. This approach improves diagnostic accuracy and patient care.
–Specialty Gases (He, Ar, etc.):
Specialty gases support advanced surgical lasers and analytical instruments. They maintain the high purity required for critical procedures. Their monitoring ensures the reliability of complex medical systems.
–Blood-Gas Analytes (pH, Electrolytes, Lactate):
Blood-gas analyzers measure pH, electrolytes, and lactate levels. These parameters assess acid-base balance and metabolic status. Accurate blood-gas data guides urgent interventions and critical care decisions.
How Do ESEGAS Gas Analyzers Integrate into Healthcare Workflows?

Here’s a concise integration table showing how ESEGAS gas analyzers map to key medical gases, their detection capabilities, and practical use in healthcare workflows:
| Medical Gas / Analyte | ESEGAS Product | Analyzer Technology & Range | Medical Monitoring Concentration | Medical Workflow Application |
| Oxygen (O₂) | Oxygen (O₂) Gas Analyzer | ECD ; 0–25 vol% (Paramagnetic); up to 100 vol% (TDLAS) | 21–100 vol% (FiO₂ in ventilators) | Continuous FiO₂ feedback in ventilators and anesthesia circuits |
| Carbon Dioxide (CO₂) | CO₂ Gas Analyzer;Portable FTIR Gas Analyzer | NDIR/TDLAS ppm–% (customizable, e.g., 0–10 vol%); 0~30%vol (customizable) (FTIR) | 0–10 vol% (EtCO₂, ABG) | EtCO₂ capnography for ventilator management and procedural sedation |
| Nitrous Oxide (N₂O) and Other Anesthetic Agents | NDIR Gas Analyzer;Portable FTIR Gas Analyzer | (0-100)mg/m3(NDIR); ppb–% (FTIR) | 0–5 vol% N₂O; 0–2 vol% sevoflurane | Anesthesia gas delivery monitoring and depth titration |
| Carbon Monoxide (CO) | CO gas analyzer | TDLAS/NDIR;ppm–% (e.g., 0–10 ppm) | <5 ppm breath CO | Breath CO testing for poisoning and smoking‐status monitoring |
| Methane (CH₄) | Methane (CH₄) Analyzer;Portable FTIR Gas Analyzer | 0–5000 ppb (min DL 5 ppb) (TDLAS);0~500ppm (customizable) (FTIR) | 0–10 ppm breath CH₄ | Breath CH₄ testing for SIBO and gut‐dysbiosis diagnosis |
| Volatile Organic Compounds (VOCs) | Not covered by ESEGAS | N/A | ppb–low ppm | Breathomics for biomarker detection (e.g., NO, acetone) |
| Specialty Gases (Helium, Argon, etc.) | Not covered by ESEGAS | N/A | >99.9% purity | Purity verification of surgical/therapeutic gases (cryotherapy, laparoscopy) |
| Blood-Gas Analytes (pH, Electrolytes, Lactate) | Not covered by ESEGAS | N/A | pH 7.35–7.45; PaO₂ 80–100 mmHg | Combine gas readings with biochemical panels in blood-gas systems |
This mapping highlights how ESEGAS’s versatile analyzer portfolio can directly address the full spectrum of gas monitoring needs in modern healthcare, from critical care ventilation to non-invasive diagnostics and medical-gas quality assurance.
What Are the Best Practices for Implementing Gas Analyzers in Healthcare?
1. AI-Driven Analytics for Predictive Alerts

(the future of healthcare)
Innovations in AI-driven analytics will help predict patient deterioration before vital signs change. By analyzing gas concentration trends, algorithms can flag early signs of respiratory distress or sepsis. Furthermore, machine learning models trained on large datasets can customize alarm thresholds for each patient. Consequently, clinical teams receive predictive alerts that guide proactive interventions and reduce adverse events. This shift, from reactive to predictive monitoring, promises to improve patient outcomes and operational efficiency.
2. Wearable & Point–of–Care Analyzers for Tele–Monitoring
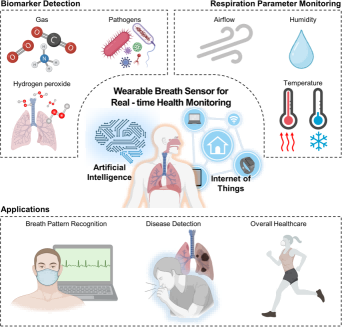
(Wearable breath sensor)
Wearable and point-of-care analyzers will bring gas monitoring beyond the ICU. Compact, battery-powered sensors can track breath biomarkers and oxygen levels in real time. Moreover, tele-monitoring platforms connect these devices to care teams remotely. As a result, patients with chronic respiratory conditions can receive continuous oversight at home. Ultimately, this approach reduces hospital visits and empowers patient self-management.
3. Integration with Omics for Precision Medicine
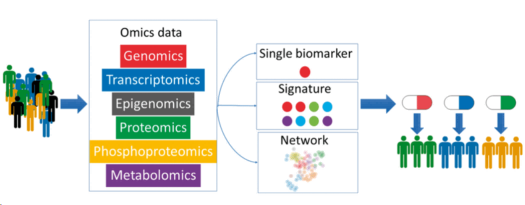
(Multi-Omics)
Integration with omics will unlock precision diagnostics and therapy optimization. By combining gas analysis with metabolomics and proteomics, clinicians can link breath biomarkers to molecular pathways. In addition, multi-omics data fusion supports personalized treatment plans and early disease subtyping. Furthermore, AI-based models can interpret complex omics-gas datasets to reveal hidden patterns. This convergence, of gas sensing and omics, heralds a new era of precision medicine.
If you have any questions, consulting with our ESEGAS team please!